5 Common Types of Knee Injuries and Treatment
This post may contain affiliate links, and we may earn compensation from qualified purchases.
Knee pain is a common complaint of people of all ages and activity levels. Conservative treatment is commonly effective, however, surgical intervention may be necessary at times. Physical therapy can help not only with treatment but prevention as well!
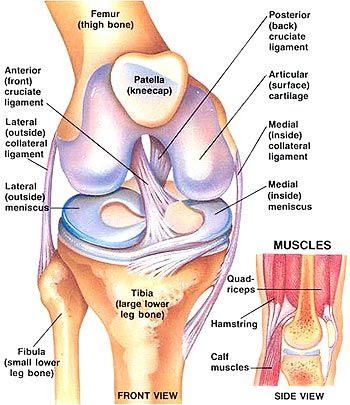
So let’s talk knees! It is important to first get familiar with the anatomy. While we always try to use layman’s terms in the clinic, sometimes we let that medical jargon slip. Don’t be afraid to ask questions if that happens; we love to be on the same page! We also love teaching and we hope you learn something new as you read on…
Here is a picture showing the anatomy of the knee. Which terms do you recognize? Have you caught us spouting medical jargon?
This picture is great because it shows both medical jargon and layman’s terms in parentheses!
Knee problems are very common and occur in people of all ages. Knee problems can be debilitating and interfere with simple activities such as getting up and down from a chair or walking, as well as more aggressive activities like exercise and sports.
Here are Five Common Knee Injuries and Treatments:
- Fracture/ Dislocation
- Ligament Sprain/ Tear
- Meniscus Tear
- Iliotibial Band Syndrome (ITBS)
- Patellofemoral Pain Syndrome (PFPS)
- Osteoarthritis
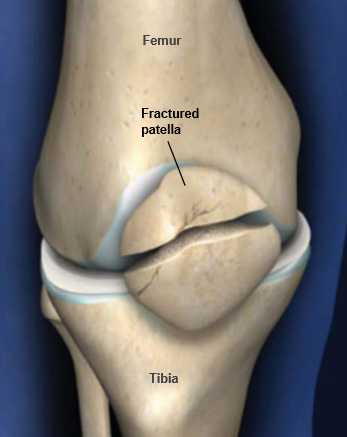
Fracture/Dislocation:
The patella (kneecap) is the most common bone in the knee that is fractured, however, you can break the femur, tibia, and fibula as well.
This can be due to sports injuries, falls, car accidents, or osteoporosis.
Ligament Sprain/Tear:
An ACL rupture usually occurs due to cutting, pivoting, planting and twisting or sudden stops. The ACL connects the femur to the tibia and helps to stabilize the knee. When injured, one commonly hears a “pop,” pain and inability to continue activity occurs, swelling is typically observed, and one may experience the knee “giving out.”
PCL, MCL, and LCL are other ligaments in the knee that can be injured.

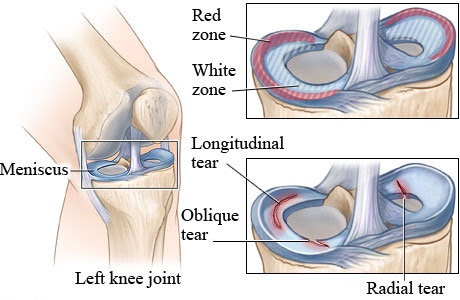
Meniscus Tear:
Meniscus tears are pretty common knee injuries mostly plaguing athletes but can occur in all populations. Menisci are cartilaginous discs between the bones that form your knee (femur and tibia) and act as “shock absorbers.”
Tears typically occur with a bend and twist of the knee. That may be due to direct contact with athletes or simply getting up from a chair or out of a car for older adults. There is typically a decreased range of motion, pain at end ranges of motion, catching or locking, delayed swelling, and the knee may “give way.”
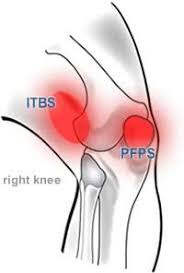
ITBS:
The Iliotibial band, aka IT band, is a thick band of connective tissue that runs
the span of the thigh from the hip to the knee. If this band rubs against the thigh it can cause irritation and pain; this is iliotibial band syndrome (ITBS).
There is the possibility of bursitis as well; bursas are fluid filled sacs that help cushion joints. There are several bursas in and around the knee that, with constant friction, can become inflamed and irritated.
PFPS:
PFPS is patellofemoral pain syndrome and is one of the most common diagnoses seen by doctors. It is most often an overuse injury affecting the cartilage under the kneecap. It is most commonly seen athletes, and women more than men.
Squatting and negotiating stairs, and prolonged sitting are typically painful activities.
Osteoarthritis:
OA typically affects aging adults. It is often progressive as the cartilage in the knee wears down over time. Bone spurs can form causing increased pain. The joints become stiff and can crack and pop making noise when moving. Weather can interfere with symptoms and joint deformity can be observed. All activities are affected, especially walking and getting in and out of chairs, etc.
The knee is a common joint affected by OA.
Unfortunately, there are more injuries that can occur to the knee. Listed above are some of the common ones we see most often. If anything you just read sounds familiar or you are experiencing something not listed above, don’t hesitate to contact us. We can help you or direct you in the right direction to find the help you need.

Treatment for Common Types of Knee Injuries
Conservative treatment for various musculoskeletal injuries encompasses a wide range of therapeutic approaches aimed at promoting healing, reducing pain, and restoring function. The several key components that can significantly contribute to the recovery process are education, soft tissue mobilization, joint mobilization, massage, tape, activity modification, strengthening, rest, ice, elevation, and medications/injections…in essence, physical therapy!




- Tape: One effective method in conservative treatment is the use of taping techniques, such as kinesiology tape or athletic tape. These can provide stability to injured joints or muscles, reduce pain by altering biomechanics, and facilitate better movement patterns during rehabilitation. For instance, kinesiology tape can help support weakened muscles, improve circulation, and alleviate discomfort. It’s often recommended for conditions like sprains, strains, or tendinitis.
- Strengthening: Strengthening exercises are a cornerstone of rehabilitation. Tailored to each individual’s needs, these exercises aim to rebuild muscle strength and endurance, thereby enhancing joint stability and preventing future injuries. For example, in cases of knee injuries, a physical therapist may prescribe exercises like leg raises or squats to target specific muscle groups and regain functional strength.
- Ice: The application of ice, also known as cryotherapy, plays a vital role in managing inflammation and pain. Ice can help reduce swelling and numb the affected area, providing relief. Products such as gel ice packs or cold compression wraps can be recommended to make the icing process more convenient and effective for patients.
- Elevation: Elevation is a simple yet effective strategy to minimize swelling and improve blood flow to the injured area. Elevating the injured limb above the level of the heart can be achieved with the help of foam wedges or pillows. Recommending suitable products for elevation can help patients maintain this crucial aspect of their home care routine.
Incorporating these product recommendations into the treatment plan can enhance the overall effectiveness of conservative therapies. It’s essential to note that the choice of products and their application should be tailored to each patient’s specific injury and needs, and should always be used under the guidance of a qualified healthcare professional to ensure safe and effective rehabilitation.
After a careful and personalized examination and evaluation, an individualized treatment plan will be created for you. We have several different techniques to help you including soft tissue mobilization, instrument-assisted soft tissue mobilization, joint mobilization, mobilization belts, cupping, deep muscle stimulator (DMS), ultrasound, compression bands, etc. Perhaps other specialties such as acupuncture or massage therapy may be beneficial (We have recommendations!). A targeted strengthening program will be developed to cater to your specific needs. Often, the above injuries can be treated conservatively, however, there are also cases in which surgery is the recommended treatment.
Fractures, ligament tears, tendon ruptures, meniscal tears, and end-stage osteoarthritis (along with other diagnoses) might have to be treated surgically. Depending on the injury and the surgery, the prognosis will vary. That’s where we come in, again! We can help you navigate the rehabilitative process after surgery. That’s our job and we love it!
More from the blog:

